MIND YOUR LIVER. IT NEEDS YOU. ™
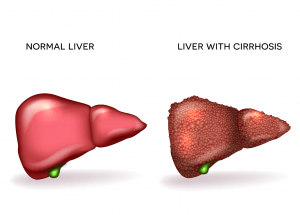
Cirrhosis is a progressive liver disease characterized by severe scarring and loss of liver function. Understanding the causes, such as chronic alcohol abuse, viral hepatitis, and fatty liver disease, is crucial for prevention. Recognizing the symptoms, including fatigue, jaundice, and abdominal swelling, allows for timely medical intervention. Exploring available treatment options, from lifestyle changes to medical therapies, can help manage the condition and promote better liver health.
Cirrhosis is often referred to as the “silent killer” of liver health due to its insidious progression and the lack of noticeable symptoms in its early stages. This chronic liver disease occurs when healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function properly. Common causes include chronic alcohol abuse, viral hepatitis, and non-alcoholic fatty liver disease. As the liver becomes increasingly damaged, it struggles to perform essential functions, such as detoxification, protein synthesis, and bile production. Unfortunately, many individuals remain unaware of their condition until significant liver damage has occurred, underscoring the importance of regular check-ups and awareness of risk factors.
As cirrhosis advances, it can lead to severe complications, including liver failure, portal hypertension, and liver cancer. Symptoms that may emerge include fatigue, jaundice, and abdominal swelling, which can significantly impact a person’s quality of life. While cirrhosis is irreversible, early detection and lifestyle modifications can help slow its progression and improve overall health. Treatment options may involve managing underlying conditions, adopting a healthier diet, avoiding alcohol, and in severe cases, considering liver transplantation. Raising awareness about cirrhosis and its risks is crucial for prevention and encourages individuals to seek medical advice if they exhibit symptoms or are at risk.
Progressive Liver Damage: Cirrhosis is characterized by the gradual replacement of healthy liver tissue with scar tissue, leading to impaired liver function. This condition can develop over many years, often as a result of chronic alcohol abuse, viral hepatitis, or non-alcoholic fatty liver disease. Early-stage cirrhosis may be asymptomatic, making regular monitoring and liver health awareness critical.
Cirrhosis can lead to severe complications, including liver failure, portal hypertension (increased blood pressure in the liver), and an elevated risk of liver cancer. Once diagnosed, individuals with cirrhosis may require ongoing medical management and lifestyle changes to slow disease progression and prevent life-threatening complications.
Cirrhosis is sometimes called end-stage liver disease. This simply means it comes after the other stages of have damage which can include inflammation (hepatitis), fatty deposits (steatosis) and increased stiffness and mild-scarring of your liver (fibrosis).
Many people with cirrhosis can feel quite well and live for many years without needing a liver transplant. This is because the liver can function relatively well even when it is quite severely damaged.
Cirrhosis is classified as compensated or decompensated.
Compensated cirrhosis is where the liver is coping with the damage and maintaining its important functions. In decompensated cirrhosis
, the liver is not able to perform all its functions adequately. People with decompensated liver disease or cirrhosis often have serious symptoms and complications such as portal hypertension, bleeding varices, ascites and hepatic encephalopathy.
There are also systems for grading cirrhosis according to its severity. One of these is the Child-Pugh score, which uses symptoms including encephalopathy and ascites together with blood test results for bilirubin, albumin and clotting, to grade cirrhosis from A (relatively mild) to C (severe), There are other systems including MELD (model of end-stage liver disease) which are used to help decide which patients most urgently need liver transplants. It uses blood test results for bilirubin, creatinine and clotting (INR).
NAFLD often presents with few or no symptoms in its early stages. However, as the disease progresses, some common symptoms may include:
These symptoms can vary in severity and may indicate the need for further medical evaluation and intervention.
As we gear up to make a positive impact, we invite you to join us on this new & exciting journey. Stay tuned for resources, support groups, workshop event dates, and engagement opportunities that empower our youth to prioritize their liver health. Join the movement and be the first to know when we launch!
Liver Awareness Foundation (LAF) promotes liver health education and alerts young people to possible liver conditions. We raise awareness of alcohol-associated liver disease and empower informed lifestyle choices to prevent liver problems. All through our founding principle: Mind Your Liver. It Needs You. ™️
All content copyright © 2024 The Liver Awareness Foundation. All rights reserved. Charity Registration Number: 719004947RT0001